Lymphoedema: what you need to know
March is Lymphoedema Awareness Month, so we are sharing information for people who have had treatment for cancer and may be at risk of developing this condition.
What is lymphoedema?
Lymphoedema is swelling (oedema) that occurs when fluid (lymph) builds up in tissues, under the skin, or sometimes more deeply in the chest, abdomen or neck. Your arms and legs are most commonly affected after cancer treatment.
When this swelling is caused by damage to the lymphatic system (for example, by surgery or radiotherapy), it is called secondary lymphoedema. In rare cases, people may develop primary lymphoedema, but we are only discussing secondary lymphoedema here.
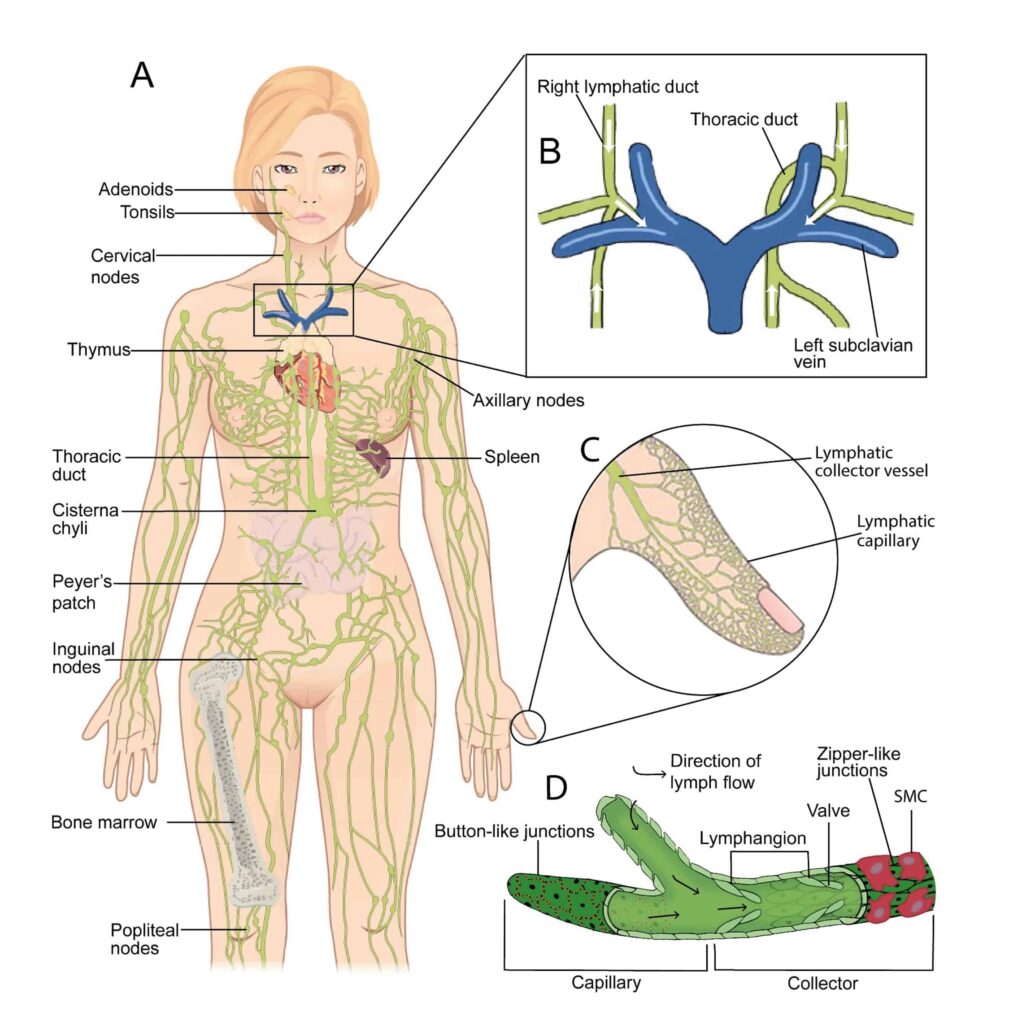
What is the lymphatic system?
The lymphatic system protects the body against infection. It is made up of a network of fine tubes across the body. It carries lymph fluid from tissues and organs and takes this to lymph nodes. The lymph nodes filter the lymph fluid removing bacteria and viruses. Then the filtered lymph fluid passes out of the lymph nodes into the bloodstream.
Who gets lymphoedema?
If the lymphatic system isn’t working properly, lymphoedema can occur at any time. For people diagnosed with cancer this can happen during initial treatment, after treatment is completed or when you’re in remission. It may develop if you’re experiencing advanced cancer. Usually it develops slowly, over many months or even years.
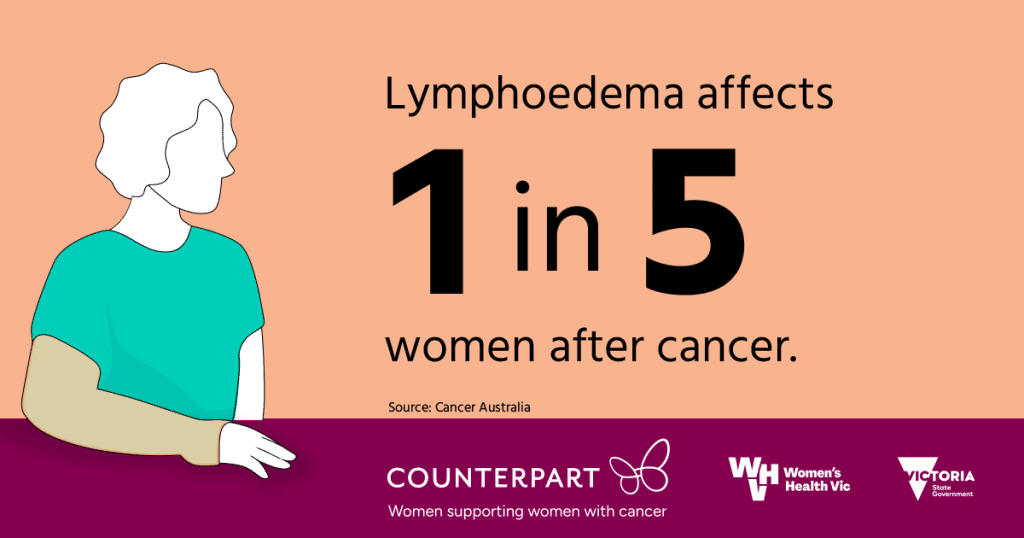
More than one in 5 people with cancer develop lymphoedema to some degree. Most don’t and it depends on the type of cancer you have, where it is, what treatment you’ve had and other health conditions you experience.
Risk factors include (from the Cancer Council, 2023):
- surgery that removes lymph nodes
- radiation therapy that damages the lymphatic system (scarring and thickening the vessels so they’re not carrying the lymph fluid as well as before)
- Taxane-based chemotherapy (speak with your oncologist about this association)
- an infection in the limb where lymph nodes were removed/damaged
- an injury to the lymphatic vessels
- obesity
- not being able to move around easily
- rheumatoid arthritis
- older age.
The table shows areas that may be affected by lymphoedema depending on the type of cancer:
| Cancer type | Commonly affected areas |
| Bladder | Genitals and legs |
| Breast | Arm, hand, breast, chest, trunk |
| Cervical | Genitals and legs |
| Head and neck | Face, below chin and/or neck |
| Melanoma | Any part of the body such as face, neck, hand, forearm, upper arm or whole arm, breast and/or chest wall, legs |
| Ovarian | Genitals, abdomen/trunk and legs |
| Uterine | Legs |
| Vulvar/vaginal | Genitals and legs |
How do I know I have lymphoedema?
Diagnosing lymphoedema early gives you the best chance of reducing how it affects you.
Early signs include:
- swelling that is soft to the touch and is usually not painful at first
- swelling and a heavy or achy feeling in your arms or legs that may spread to your fingers and toes
- swelling and a tight uncomfortable feeling on your face, neck, or under your chin
- difficulty moving your head or neck
- a dent when you press on the swollen area
- tight watches, jewellery or clothes.
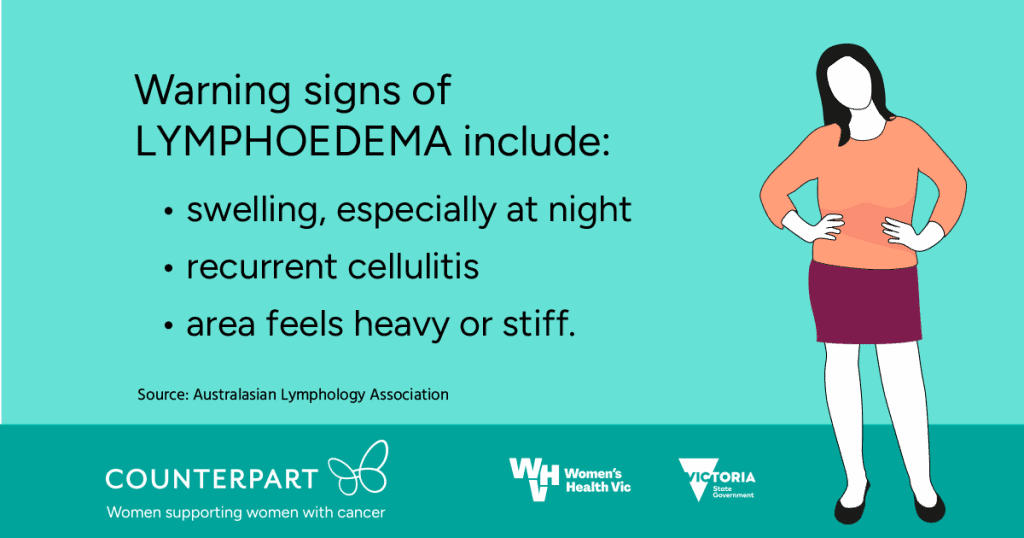
Later signs include:
- swelling that doesn’t go down after elevation (overnight)
- swelling that is firmer and more difficult to dent
- infection – cellulitis (redness, heat and pain) of the skin over the swollen area
- nail changes to the affected limb.
What help can I get?
Treatment improves the lymphatic fluid’s flow through the affected area. This helps reduce swelling and improves the health of the swollen tissue. Reducing the swelling will lower your risk of infection, make movement easier and more comfortable, and improve your wellbeing. A range of health professionals may be involved in your care including a lymphoedema practitioner, your doctor, a podiatrist and dietitian.
Treatment can include:
- skin care, especially preventing infection, including nail care
- exercise, moving the affected area helps move the lymphatic fluid
- maintaining a healthy weight
- massage therapy (manual lymphatic drainage, if needed)
- compression therapy (if advised).

If you talk to your doctor about getting a Management Plan, you can be referred to an Accredited Lymphoedema Practitioner and may be eligible for Medicare rebates for up to five sessions from approved allied health professionals. You can also ask your oncology team about what services are available.
More information
Australasian Lymphology Association (ALA) (lymphoedema.org.au) The ALA is a professional association for lymphoedema practitioners and those working in or interested in lymphoedema. Their website includes information and a look-up tool to help you find an accredited practitioner near you.
Lymphoedema Association Australia (www.lymphaustralia.org.au) The Lymphoedema Association provides information and support to people living with lymphoedema.
Counterpart webinar recording: Lymphoedema (recorded 6 March 23)
Counterpart webinar recording: Self care for lymphoedema (recorded 9 March 22)
Understanding Lymphoedema (cancervic.org.au) (Cancer Council Victoria)
Physiotherapy and Lymphoedema (headandneckcancer.org.au) Information about lymphoedema as a result of head and neck cancer.
Counterpart's ovarian cancer Navigator: lymphoedema
Counterpart's breast cancer Navigator: lymphoedema